GPNewsFlash – January 2018
Categories: GPNewsFlash
- Contemporary Management of Combined Lip Puncture and Dental Trauma
- Hands-on Oral Surgery, 3D Printing, and the Unstoppable Team
2018 CAGD Annual Meeting - Anatomy of Data Breach in the Dental Office:
Just Uncomfortable or Catastrophe - Oral Health Literacy: Its Importance to All of Us and What We Can Do About It
- Congratulation to Dr. Michael Lew of Novato, California!
The AGD Secretary, 2017-2018 - CAGD’s GPNews (printed newsletter) May and September 2017 Issues are Available Online
Contemporary Management of Combined Lip Puncture and Dental Trauma
Autologous collection of blood concentrate products (CGF and Fibrin membrane) to promote soft tissue healing in combined soft tissue and dental trauma

Dr. Nora Vinh
By Nora Vinh Svihl, DMD
California AGD Mastertrack-5
Private General Practice, Fountain Valley, CA
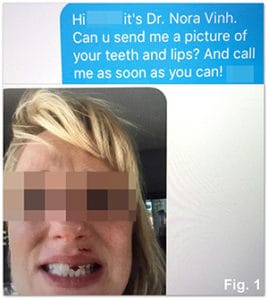
Text message of lip and dental injuries received from patient on a holiday afternoon.
Receiving an emergency phone call on a holiday afternoon, followed by a text showing a photo of a patient-of-record with some sort of extraoral laceration to her upper left lip and several broken upper and lower anterior teeth will definitely put your adrenaline glands to work (Fig. 1). Dental trauma to the esthetic zone presents unique challenges especially in the esthetically conscious patients. Fortunately, I was in town and my lead dental assistant was also able to report for duty.
Findings and Diagnosis:
The patient was removing a large, heavy box filled with metallic auto parts from a high shelf and the corner of the box hit her lip and broke some teeth. She had not been unconscious nor experienced any central symptoms, and she experienced full range of movement in her neck and shoulders. In the absence of these symptoms and other apparent mobile facial fractures, her main concerns were limited to the fractured teeth, punctured lip, and tooth pain, which she described as throbbing and shooting.
The upper left lip had a puncture laceration with small jagged borders 1 cm in length (Fig. 2). The laceration exited into the inner lip mucosa as a through and through puncture, with the exit wound having significantly more enlarged, complex borders and diffuse swelling.

Pre-op findings: Fig. 2: Lacerated outer lip. Fig. 3: Fractured #9.
Fig. 4: Fractured # 23 & #24.
Tooth #9 was the most injured tooth, with a very clean shear horizontal fracture of almost half the crown and with damage to the attachment apparatus (Fig. 3). The fracture was just barely above the pulp chamber, with no pinpoint exposure present. The tooth was sensitive to palpation, percussion and room air and most likely her pulpal symptoms were a result of acute pulpitis. Palpation of the alveolus looking for movement and periapical x-rays revealed no significant findings.
Teeth #’s 23 and 24 had corner uncomplicated fractures, limited to the incisal enamel and had no mobility or pulpal symptoms (Fig. 4). The joint exam was significant for pain upon trying to close fully into maximum intercuspation where the patient could barely hit the anterior teeth.
Emergency Treatment: Stabilizing the Injuries
Soft Tissues
Profound anesthesia was attained with plain carbocaine without epinephrine slowly injected intraorally around the lip tissue and with intraoral apical facial infiltration over the course of treatment. The soft tissue wounds were flushed thoroughly with copious amounts of sterile saline to remove debris. The skin around the lip area was cleaned with sterile 4×4 gauze and alcohol.

Immediate Post-op: Fig. 5: Sutured lacerated outer lip. Fig. 6:
Sutured inner lip. Fig. 7: Temporary crown tooth #9.
Extraorally, a 6-0 PFTE (Cytoplast) continuous horizontal mattress suture and two simple interrupted sutures at each end of the wound were placed through the skin and underlying muscle to closely approximate the edges (Fig. 5). All sutures were tension free, and suture lines were away from the laceration. Internally, the same sutures were placed in single sutures to approximate the deep tissues of the lip and a continuous figure 8 suture to closely bring the jagged edges as close as possible (Fig. 6). At every step of suturing the internal aspect, the skin approximation on the outer lip was referenced to make sure the edges were tightly approximated without tension, pulling, or rolling.
Additionally, two vials of blood from the patient’s right antecubital fossa were withdrawn to retrieve concentrated growth factors in liquid form (white vial) to flush the wound sites and fibrin membrane form (red vial) to be integrated into the inner lip wound to promote healing in a procedure known as autologous collection and creation of blood concentrate products. Using a specially designed medi-fuge (Neobiotech, Silfradent) and designated proprietary vials designed to separate the blood into its white versus red elements, the patient’s own concentrated growth factors containing VEG-F, endothelial growth factor, PDGF-1, TGF-β and platelet-rich fibrin were inject into the wound site, which also had the immediate benefit of hemostasis.1
This technology has widespread advantages for dentistry such as faster and less painful surgical healing, promotion of bone graft placement (sticky bone), and the treatment of dry socket. There is also anecdotal evidence for its use in periodontal pocket reduction. 2 It is the author’s experience that all patients are very comfortable with phlebotomy, albeit intrigued and curious about its uses in their dental treatment. However, they are all amenable to it if it is advantageous to their postoperative recovery, and indeed, most users of this technique in adjunct with periodontal and even endodontic procedures have seen a marked decrease in the need for prolonged opiate pain management regimens and post-operative swelling, pain, and a much faster biologic healing than without. The most common barrier is the need to learn basic phlebotomy techniques. Dentists can receive training in this technique at many courses offered over a weekend. However, in the cases where patients have difficult blood draw experiences such as in patients who have received I.V. chemotherapy, have collapsible/fragile venipuncture history, have large amounts of adipose tissue hiding the veins, and are chronically dehydrated, the dentist may hire the services of a licensed phlebotomist.
Hard Tissues
The periodontium of tooth #9 was gently irrigated with copious chlorhexidine. A wax up was done intraorally using composite to recreate the original contours as a rough guide for a provisional impression. The tooth was prepped for a full coverage all ceramic crown and the provisional was polished and given characterization with white opaquer (Fig 7). Teeth #’s 23 and 24 were restored with direct composite restorations. No impression of tooth #9 was taken at this emergency visit until the periodontium would heal for at least another 3-4 weeks, and manipulation of the lip could then be done.
Post-op Care Instructions
Since the patient was allergic to Amoxicillin, Clindamycin 300 mg x30 one q6h was prescribed to help reduce the risk of any post-trauma infection that would compromise healing in such a critical site. Motrin 600mg one q6h prn was prescribed to reduce the swelling while also alleviating post-trauma discomfort. It was stressed to the patient that she should avoid excessive laughter or movement of the upper lip area for ten days if possible. Wound cleansing protocol was given for home with warm salt water and gentle liquid soap, and absolutely no make-up or creams, as well as avoidance of sun exposure. Immediately after emergency dental treatment (which took five hours total), the patient went to the Hospital Emergency Department and was cleared of facial and cervical spine fractures. TMJ symptoms were not resolved during emergency dental treatment; but they would be treated over the next 6 months.
Follow-up of Soft Tissue Healing
The patient continued to follow up over the course of the next three weeks as her lip healed. Dialogue consisted of photos of the lip sent by the patient via email, as well as photos taken at our dental office. The patient was advised to use an antibiotic ointment (Neosporin) on the outer lip on top of the sutures which she applied with a new Q-tip every day (Fig. 8). By the middle of the second week, skin edges were clean and approximating and it was clear that there would be no raised scar (Fig. 9). By the end of the third week, the sutures were removed gently (Fig. 10) and tooth # 9 was ready for final impression.
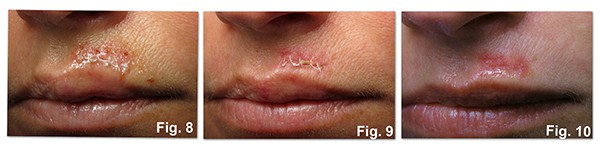
Extraoral lip post-op healing. Fig. 8: Two days post-op with antibiotic ointment. Fig. 9: Ten days post-op. Fig 10: Three weeks post-op, immediately after suture removal.
Final Restorative Treatment

Final results, 11 weeks post-op. Fig. 10: Full face with smile.
Fig 12: Final restorations teeth #’s 9, 23, & 24.
The patient’s centrals had myriad white spots, greyish translucency, and a slight pebbly texture. She was sent to a dental laboratory (Dentech, Irvine CA) to consult with the technicians who took their own photographs and custom shade tabs. The restoration of choice was translucent zirconia core fused to porcelain with internal live stain technique, and it was cemented 11 weeks post injury. This time also allowed ruling out endodontic referral, as the teeth had been testing vital to endodontic tests, without symptoms of pulpitis. However, it took 6 months for TMJ symptoms to resolve. Treatment was completed over 1 year ago, and the patient continues to be asymptomatic and happy with the esthetic result (Fig 10-12).
Dr. Vinh presented this case to her peers at the California AGD MasterTrack-5 as a part of the educational requirements for Mastership in the Academy of General Dentistry (MAGD).
The author has no financial, economic, commercial, and/or professional interests in any of the companies whose products or devices are included in this article.
Dr. Vinh may be reached at [email protected] or (714)962-1300
References:
1. Naik B, Karunakar P, Jayadev M, Marshal VR. Role of Platelet rich fibrin in wound healing: A critical review. J Conserv Dent. 2013;16(4):284-93.
2. Simonpieri A, Del Corso M, Vervelle A, Jimbo R, Inchingolo F, Sammartino G, Dohan Ehrenfest DM. Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 2: Bone graft, implant and reconstructive surgery. Curr Pharm Biotechnol. 2012;13(7):1231-56.
____________________________
Hands on Oral surgery, 3D Printing, and the Unstoppable Team
Join Us for the 2018 CAGD Annual Meeting in Newport Beach on
Saturday, Jan 26th

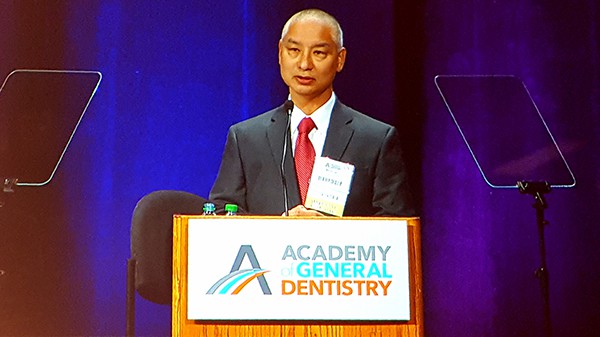
California general dentists listening to Dr. Karl Koerner’s lecture about oral surgery (left) and sharing how to overcome the challenges of everyday general practice over a fellowship lunch (right) at the CAGD Fall Meeting on Oct 28th, 2017 in Newport Beach.
Join us at the 2018 CAGD Annual Meeting and learn proven hands-on surgical skills and 3D printing, build a successful and empowered unstoppable team, increase your practice revenues, or simply discover innovative services and products while networking with like-minded colleagues in a relaxing atmosphere.
Course 1: Building Surgical Skills (8 hands-on CE) – Dr. Karl Koerner, limited to 40 attendees
Course 2: The Unstoppable Team – Jonathan Miller, A fortune Management Executive Coach
Course 3: Intro to 3-D Printing for Dentistry – Dr. Kelliny
____________________________
Anatomy of Data Breach in the Dental Office
Just Uncomfortable or Catastrophe

ACS Technologies, LLC.
Dental Technology Solutions
Santa Rosa, CA
You’ve had a data breach. Ugh! As the inevitable panic sets in, where do you start?
First, take a deep breath. This will be long and complicated, with many possibilities for error, so work with a clear head and make deliberate choices.
Let’s make sure this is truly a data breach. Not all self-diagnosed “breaches” end up being a breach. If your office was broken into and computers and charts are missing – that’s pretty obvious. A patient’s complaint, an employee’s threat to disclose violations seen or even a case of downloaded ransomware may not be a reportable data breach. Engage both your IT Provider and a HIPAA data breach consultant or HIPAA attorney to determine the next steps. Fear and not knowing the truth often lead to unnecessary panic in these situations. Under no circumstances should you ignore this or sweep it under the rug. The truth always comes out and your patients will crucify you if they found out you waited to tell them about your breach, or worse, warned them of a breach of their data, when in fact, their data was not compromised.
Time is of the essence. If it does turn out to be a true data breach, then you have a finite amount of time to do a long list of things. Federal HIPAA laws require notification to Health and Human Services Office for Civil Rights (OCR) as well as patient within 60 days, while some states have additional time requirements. For example, California requires notification to patients and the State Office of the Attorney General within 15 days.
Check your insurance policies. If you have data breach and cyber lability coverage and cybercrime coverage, you may have some financial protection. It is relatively new in the world of insurance and most carriers have low limits or exclusions such as legal representation for civil (patient) lawsuits, viruses, or malicious codes. A good rule of thumb is for every 1,000 charts (both active and inactive) you have, you should carry $500,000 of insurance. If you do have this insurance, it’s wise to put your carrier on notice as soon as you know for sure you are dealing with a reportable breach.
Forensics. Next is bringing in the forensic computer people. You can shout your claims from the rooftops, but unless a forensic company writes and signs off on the report, it doesn’t count. Be prepared to pay a lot for this one. Forensics start around $5,000 for moderate investigations.
Legal counsel. At the same time you should engage a HIPAA data breach attorney to protect the forensic data as “discovery” under client/attorney privilege. Good attorneys have been specialized in data breaches for at least 5 years and will ensure you follow the right path. They will help with notification to state and federal agencies, negotiate any potential fines or penalties that might be imposed and help with follow up reviews as part of a resolution agreement. Most firms require a $10,000-$20,000 retainer and I’ve seen upwards of $100,000 in legal fees in extensive breaches.
Notification is next. In the event of physical theft, you often are relying on backups to access your data. Then you have to get the data set from a specific date range. Most dental practice management programs do not currently have an easy way of doing this, leading to many hours of manual work by office managers and front desk staff. I always recommend that a service be engaged to send notification to effected patients. They will set up an 800 number (so patients don’t inundate your front desk and try to make financial deals), as well as offer credit monitoring (not everyone will accept, so this cost varies) in addition to physically mailing letters to patients. And no, you cannot email this notification. Average notification costs range from $1.85-$5.75 per person.
Credit cards, press release & lawsuits. In addition, if credit or debit cards were involved in the breach, you must cover the cost to replace them (roughly $10 per card). In addition, you must do a press release. If the breach affected under 500 patients, then the press release must be done via local newspapers, while over 500 patients effected requires TV media coverage. Media coverage in addition to mail notification often leads to patient civil lawsuits. Some states have Private Right of Action Laws, which allows patients who can’t sue you for violating HIPAA itself to sue you on a state level and cite HIPAA that you were negligent and failed to secure their patient data. All of this leads to a giant headache if not done correctly.
Resolution agreement. As part of the resolution agreement, or ‘to-do list,’ you will be required to prove you have addressed the original cause of the breach as well as comply with all other reasonable and appropriate aspects of HIPAA for you practice(s). Often this means upgrading technology, improving your physical and technical security, hiring consultants to upgrade manuals and paperwork and buying equipment.
What will it cost? Depending on what you have done for HIPAA prior to your data breach, you may have a few tweaks to improve or you may have a massive overhaul to your practice and how you handle Protected Health Information. An average dental practice spends $30,000 $40,000 over a few years to get compliant.
Whoa…
While that may seem like a huge number, the bulk of that is necessary for other parts of your practice, such as computers and network equipment, IT security and physical security of your practice. If you wait until a breach happens, you could face hundreds of thousands of dollars; and that is if you’re lucky and don’t get fines or lawsuits. According to Netdilligence the average cost of a data breach claim to insurance is $665,000! This is accurate for a 5 operatory practice with 10 employees.
The good news is that while OCR does impose fines on egregious violations and make public examples of them, OCR silently closes out many resolution agreements every year when those Covered Entities adhere to the improvements in their resolution agreement. Bottom line – if you do what you’re supposed to do anyway, there’s a strong likelihood it will just be uncomfortable instead of catastrophic.
Amy Wood is a HIPAA Data Breach Mitigator specializing in making dental practices compliant and secure. She is president of ACS Technologies, LLC, a Northern California HIPAA Compliance & IT firm. Amy has written many articles for various dental publications and spoken at dental associations, study clubs and private practices. She runs ACS with her husband, Scott and lives in Santa Rosa, CA with their three daughters. She can be reached at [email protected]
Oral Health Literacy: It’s Importance to All of Us and What We Can Do about It

Dr. Mike Bromberg of Reseda, California leading the Oral Health Literacy Panel held during the AGD House of Delegates Meeting in Chicago on November 4th, 2017
The Healthy People 2020 midterm report indicated a decline in the number of people who visited the dentist in the last year. It should also be noted that even those with dental insurance, only 60% take advantage of their benefits. A recent study in Washington State found that the hospital emergency room was the first dental visit for 1 out of every 4 children overall and roughly half of the children younger than 3.5 years old. Many of the mothers interviewed at the emergency rooms indicated that when baby’s used a bottle at bedtime, often it was filled with Mountain Dew, Coca Cola, apple juice or some other highly sugared inappropriate liquid. Hence, tooth decay related hospital room visits are costing hundreds upon hundreds of millions of dollars, saddling the states with some of these expenses through Medicaid and other public programs. Additionally, there are many patients with dental insurance who need to take advantage of their benefits. This is where oral health literacy becomes very crucial.
Oral Health Literacy is “The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate oral health decisions.”
On April 24, 2015, the AGD brought together designated representatives of a diverse group of 10 organizations to hold the AGD’s first Oral Health Literacy Symposium. In 2016, the AGD House of Delegates adopted the OHL Consensus Statement endorsed by the American Academy of Family Physicians (AAFP); American Association of Women Dentists (AAWD); American College of Dentists (ACD); and Special Care Dental Association (SCDA):
“Oral health literacy is an integral component of every individual’s health and wellbeing. The undersigned organizations recommend addressing this critical issue in accordance with the following principles:
1. Oral health literacy is the foundation of a lifetime of wellness and must be integrated into all educational and wellness programs.
2. Oral health literacy is a shared responsibility across all sectors.
3. Critical to the advancement of oral health literacy is an established dental home.
4. The dental profession will lead the advancement of oral health literacy, in collaboration with other health professionals.
5. Governmental and private resources dedicated to improving oral health should be strategically directed toward programs that further oral health literacy.”
The AGD has also called earlier for following actions:
- Pursue development of a comprehensive oral health education component for public 9 schools’ health curriculum in addition to providing editorial and consultative services to primary and secondary school textbook publishers;
- Provide exams for one-year-old children as part of the recommendations for new mothers to facilitate early screening;
- Equip teachers at various levels with creative educational tools, including educational videos, puzzles, word searches and experiments that show children the value of their 15 teeth and how to care for them;
- Train daycare providers and school nurses on the importance of oral health, including on proper nutrition;
- Provide dental information to pediatricians regarding use of bottled water, fluoride, 19 fluoride varnishes, and appropriate diets;
- Provide multi-factorial interventions and educational programs to parents of young children, including through public media and information provided at hospitals and other healthcare points of care.
____________________________
Congratulation to Dr. Michael Lew of Novato, California! The AGD Secretary, 2017-2018
____________________________
CAGD’s GPNews (printed newsletter) May and September 2017 issues are available online
The GP News features clinical articles, upcoming and past CE course details, advocacy updates, news and events of the CAGD, local components, and student Fellowship tracks at all California dental schools.
____________________________
The statements expressed in this newsletter do not necessarily reflect the opinions of the California Academy of General Dentistry (CAGD), nor do they imply endorsement by the CAGD.

Robert Hubbert, DDS, MAGD CAGD
Editor-in-Chief

Samer S. Alassaad, DDS, FAGD
GPNewsFlash Editor