Surgical and Non-Surgical Management of Third Molars
Categories: Featured Articles
by Ho-Hyun (Brian) Sun, DMD, MS https://peninsulaoralsurgerysanjose.com/provider/h-brian-sun-dmd-ms/
The third molar (M3) or “wisdom tooth” can be a treatment dilemma for many practicing dentists. Not all third molars require removal but delaying treatment of those indicated for extraction may lead to complications including pain, caries, pericoronitis, infection, and/or formation of odontogenic pathology. Studies show that a small majority of impacted teeth result in a pathologic process, including an 8.6% that result in cysts or tumors.[1] In fact, a review by the UK National Institute for Health Research (NIHR) indicated that prophylactic removal of M3s could be associated with overall improvements in health-related quality of life.[2]
Detailed examinations are necessary to ascertain M3 emergencies including those with fevers, swelling, heavy purulence, or difficulty breathing, which should not be treated without the appropriate training. The most common third molar pathology however is pericoronitis, which is typically limited to the mucosa immediately surrounding the M3 and rarely threatens the airway. Pericoronitis is an inflammation of the surrounding gingiva and operculum from food or bacterial impaction around a partially erupted crown. What we often do not consider is that symptomatic pericoronitis can often benefit from treatments by the general practitioner even before referral to a specialist, especially if the patient is not able to see an oral surgeon within the next few days.
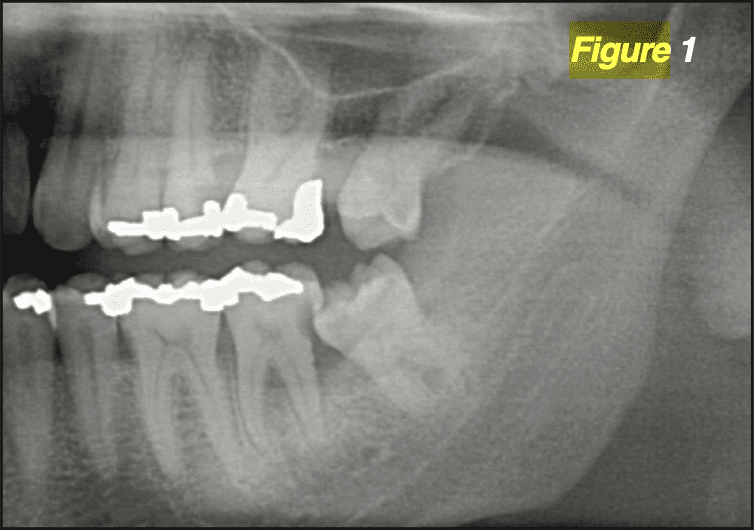
The most conservative intervention is direct application of 0.12% chlorhexidine into the second and/or third molar sulci (D9110) which helps reduce the bacterial load. When the M3 is at least partially visible, the treating dentist could further debride the impacted materials by scaling and root planning thoroughly around its crown and under the operculum (D4342). The provider must also take care to scale around the distal portion of the second molar (M2) as well, which can incur caries and periodontitis from the bacterial presence (Figure 1). Studies have indicated that deposition of minocycline microspheres (D4381) like Arestin® or Periocline® into the pericoronal pockets may afford improved control of the subgingival bacteria as well.[3]
Dentists comfortable with a blade may instead elect to remove the operculum and/or the pericoronal gingiva (D7971) completely. This helps eliminate the areas of impaction, which can provide several weeks of relief before the soft tissues often re-grow. Excision must be done with care, as incisions too far posterior can injure the lingual nerve. Some surgeons find it helpful to excise in a circular pattern with the aim of uncovering the crown without exposing the surrounding bone. All providers should expect a degree of bleeding from removal of the inflamed mucosae, which can be ad- dressed via cord packing, injection of epinephrine-containing anesthetics, local pressure, suturing, and/or the use of cauterizing agents like silver nitrate.
Patients should undergo outright removal of the M3s if other lesions are present or once pre-extraction measures have taken place. These procedures are infrequently considered “simple extractions” (D7140) especially in the mandible. Removal of even a fully erupted M3 often re- quires flap exposure through sulcus incisions (D7210) because of its positioning. For unerupted teeth, the clinician should be mindful of the degree of radiographic impaction: soft tissue (D7220), partial bony (D7230), and completely bony (D7240) impacted teeth show 0%, less than 50%, and 50% or more of the crown covered by bone, respectively. Teeth closely associated with the sinuses or the inferior alveolar nerve (IAN), or those with unusual patterns of impaction (i.e. impacted canines) may be considered completely bony impacted with unusual surgical complications (D7241). The surgeon should also carefully consider coronectomy (D7251) – removal of all crown and the coronal 3-5mm of the root – for cases with roots closely approximating the sinuses or the IAN. Coronectomy is not without its own risks but has been associated with long term resolution of pericoronitis with minimal risks to the periapical structures.[4]
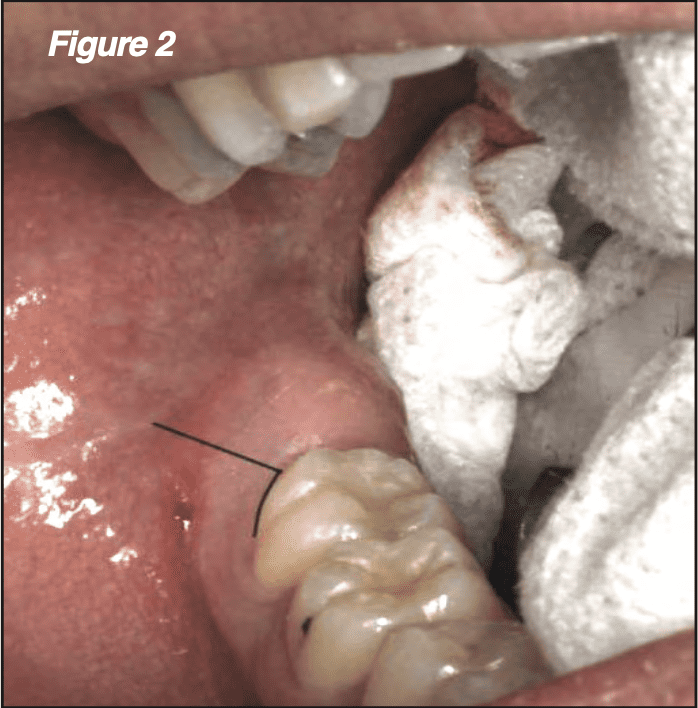
All impacted teeth should be approached with the anatomy of nearby critical structures in mind. For one, different portions of the lingual nerve rest within the retromolar trigone in approximately 20% of all patients and medial to the mandibular lingual cortex in virtually all patients. The flap design should also provide an adequate view of the third molar site while minimizing the risks of dehiscence and alveolar osteitis. We employ the mesial papilla-sparing marginal incision (MPMI), which limits the incision to the M2 buccal sulcus and a distobuccal release over the mesiobuccal portion of the M3 crown (Figure 2). Incisions through the buccal sulcus of a single tooth heal rapidly, and a distobuccal releasing incision helps ensure that the retromolar trigone is not violated.[5] In removing impacted maxillary M3s, the relative absence of critical structures allow for the use of a direct crestal incision immediately posterior to the M2.
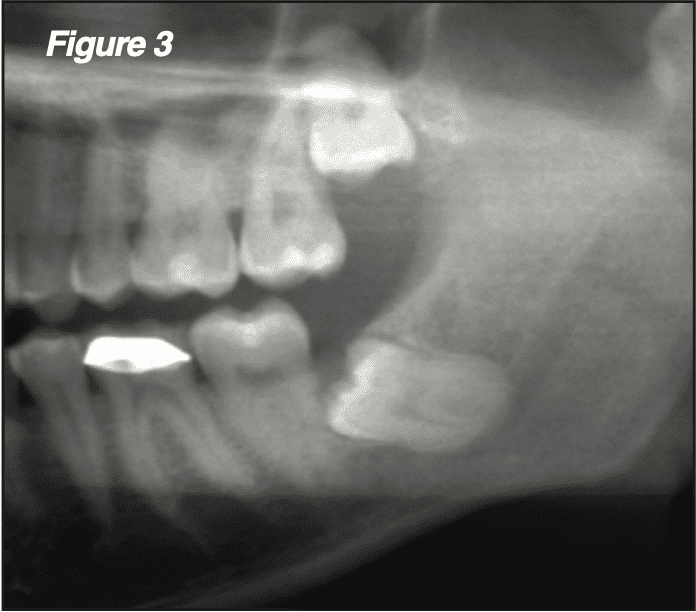
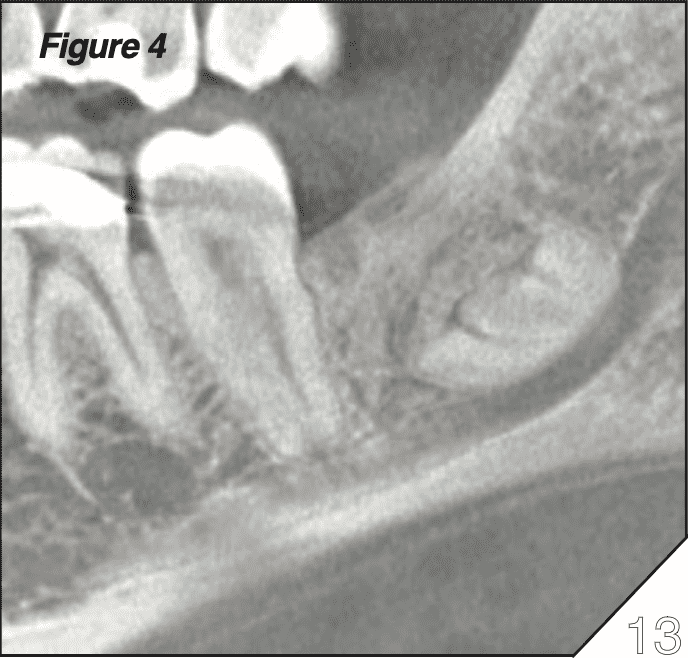
Partial or complete removal of an impacted mandibular third molar in patients aged 25 and older can result in a lingering periodontal defect posterior to the M2 (Figure 3). This defect has been associ- ated with sensitivity and mobility of the M2, and a 5+ year follow up demonstrates that this may be improved via socket grafting (D7953) concurrent with M3 extraction or even coronectomy.[4] We have utilized particulate 50/50 corticocancellous autografts to good effect in preventing these defects even in patients who M3 surgery (Figure 4).
All in all, even those without interest in surgery may be able to contribute to the care of symptomatic M3s, especially when the patient is unable to make a prompt visit to the oral surgeon. Many if not most of the symptoms arise from pericoronitis, which may be ameliorated via chlorhexidine irrigation (D9110), scaling debridement around the impacted tooth (D4342), deposition of minocycline microspheres (D4381), or a simple excision of excess pericoronal gingivae and operculae (D7971). Those with surgical proficiency should also re- main mindful of the different classification of M3 procedures from erupted surgical (D7210) to soft tissue impacted (D7220), to partial bony impacted (D7230), to full bony impacted (D7240) extractions with special considerations for the locations of the sinuses, lingual nerve, and the IAN (D7241). Furthermore, bone grafting (D7953) may be a viable option to help address periodontal defects that frequently occur from M3 surgery in individuals beyond the age of 25.
It is important to note that this article is not meant to be a definitive guide to medical or dental treatments, but to showcase common treatments considered at our practice for the treatment of third molars. Sample CDT codes have also been provided as a reference, although a billing specialist should be consulted to ensure applicability of the codes for each case.
Ho-Hyun (Brian) Sun, DMD, MS
Dr. H. Brian Sun is a Clinical Instructor and FellowTrack advisor at the University of the Pacific, a Clinical Assistant Professor at the Western University of Health Sciences, and a private practice surgeon at Peninsula Oral Surgery San Jose. He can be reached at his office on 2025 Forest Avenue, Suite 6, San Jose, Californa 95128 or by email at [email protected].
- [1] Sarica I, Derindag G, Kurtuldu E, Naralan M, Caglayan F. A retrospective study: Do all impacted teeth cause pathology? Nigerian Journal of Clinical Practice. 2019;22(4):527–33.
- [2] Hounsome J, Pilkington G, Mahon J, Boland A, Beale S, Kotas E, et al. Prophylactic removal of impacted mandibular third molars: a systematic review and economic evaluation. Vol. 24. 2020. p. 30.
- [3] Matesanz-Pérez P, García-Gargallo M, Figuero E, Bascones-Martínez A, Sanz M, Herrera D. A systematic review on the effects of local antimicrobials as adjuncts to subgingival debridement, compared with subgingival debridement alone, in the treatment of chronic periodontitis. Journal of Clinical Periodontology. 2013;40(3):227–41.
- [4] Elo JA, Sun HH (Brian), Dong F, Nguyen K, Zakhary K. Does Bone Grafting Improve Outcomes in Coronectomy Surgery? Long-Term (5- to 9-Year) Clinical and Radiographic Follow-Up of 78 Adult Patients. Journal of Oral and Maxillofacial Surgery. 2017;75(7):1330–7.
[5] Elo JA, Sun H-H (Brian), Dong F, Tandon R, Singh HM. Novel incision design and primary flap closure reduces the incidence of alveolar osteitis and infection in impacted mandibular third molar surgery. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2016;1–10.